What Is Herd Immunity, and Why Is It Important for COVID-19 Survival?

In the wake of the coronavirus pandemic, many experts have noted that herd immunity is what is needed for us to slow the COVID-19 infection rate and prevent the overwhelming spread of the disease. But there tends to be some misunderstanding about what herd immunity is. At its most basic level, herd immunity is achieved when a high enough percentage of a population has become immune to a virus, making it very difficult for that pathogen to spread from person to person. Trying to create herd immunity, though, is where things get complicated.
There are two main ways to achieve herd immunity. The first is that a large enough percentage of a population must contract a disease and either die from it or develop immunity to future infections after surviving the illness — preferably the latter. The second is that pharmaceutical companies produce a vaccine that is distributed to at least 70 to 90% of the population, and that vaccine makes them immune to the virus for a period of time.
Now that several COVID-19 vaccines are being administered around the globe, the hope is that enough people will opt to receive these immunizations — allowing us to achieve herd immunity and greatly slow the spread of the virus. However, experts are also noting that there’s a possibility herd immunity may not be achieved, and we may need to learn to live with the virus. But what exactly is herd immunity, and why is it so important?
How Herd Immunity Ended the 1918 Spanish Flu Pandemic
How helpful is herd immunity, exactly? It’s in part what ended one of the most famous pandemics in recent history: the Spanish flu of 1918. At that time and for the next year or so throughout the demobilization process, soldiers were returning home from WWI, and this travel largely contributed to the spread of the virus around the globe. The Centers for Disease Control and Prevention (CDC) estimates that at least 50 million people died due to this pandemic, and the H1N1 virus that caused the Spanish flu is believed to have infected 500 million people globally — a third of the world’s population at the time. This widespread nature of infection — the fact that so many people contracted the virus and had to either heal or die from it — was enough to create collective immunity to the virus. Interestingly, the virus has never gone away completely; remnants of the Spanish flu are still found in modern strains, even though vaccines increase our immunity to it.
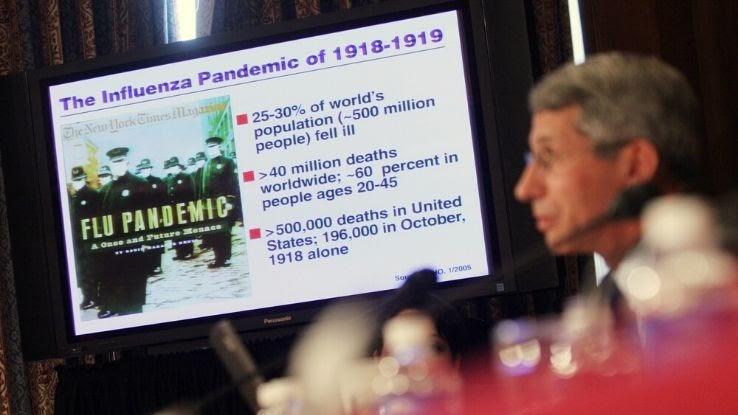
One contributing factor to why society was able to build up collective immunity to the Spanish flu is that the virus killed off a large percentage of the world’s population, and those who did survive the virus became immune. As more people became immune, the spread of the virus slowed to the point that the pandemic ended. Due to a lack of understanding of infectious diseases at that point in history, the virus was able to spread in ways we now consider preventable thanks to our modern medical knowledge, but it still stands that increasing immunity is one of the best ways to stop a pandemic.
Can We Prevent the Same Loss of Life Now?
In today’s climate with the novel coronavirus continuing to spread rapidly, health experts have been attempting to avoid the same massive loss of life the world experienced a century ago. In the case of that Spanish flu pandemic, herd immunity was achieved in two years, but it’s important to remember that it also caused many people to die in the interim. Medical professionals and health organizations now have been aiming to prevent such large-scale mortality and spreading of the virus — we have the know-how to do so this time around, despite much initially remaining unknown because of the novel nature of the coronavirus. The rapid formulation, testing, emergency approval and deployment of the vaccines that are now becoming more widely available is a testament to this.

It was initially unclear whether a single exposure to COVID-19 would be enough to build herd immunity due to the short length of time scientists believed antibodies would stay present in people who have recovered from the virus. However, despite early research suggesting that someone who has recovered from the virus may only stay immune for a matter of months, newer studies are indicating that immunity may actually last years. The vaccine that pharmaceutical company Pfizer and Oxford University developed was initially shown to create three times the number of protective antibodies than actually contracting the virus and recovering does. This may go a long way in preventing the high death toll seen with the Spanish flu a century ago.
There are several reasons why it’s likely we will be able to prevent a similar loss of life during this coronavirus pandemic. The medical community knows much more about viruses than it did during the Spanish flu pandemic; 100 years ago, technology to detect viruses didn’t exist, and scientists were only able to isolate larger bacteria. In addition to having no virus-specific diagnostic tools, medical professionals weren’t very well equipped to invent and test vaccines for viruses. Doctors ultimately ended up mixing their own proprietary vaccines with the hope that they might target the correct pathogen, and aspirin was also overprescribed to the point that it began poisoning people. Needless to say, things are different now. We’ve learned much about viruses and bacteria over the last 100 years.
So far, explains the BBC, today’s coronavirus pandemic is much less deadly than the Spanish flu outbreak of 1918 was. Interestingly, we’re still applying some of the techniques now that were used to slow the spread of the flu virus back then. In response to the Spanish flu, many large cities closed high-traffic spaces and businesses like theaters and schools, and they also banned large gatherings of people. Masks became mandatory in some cities like San Francisco, where people were charged a $5 fine (about $85 when adjusted for inflation) and charged with disturbing the peace if they were caught not wearing masks. The fact that we’re still practicing these activities to prevent the spread of the coronavirus today speaks to their efficacy — but people need to continue practicing them.
Vaccines and Herd Immunity
A likely pathway to herd immunity for COVID-19 comes by way of vaccines, which is how we’ve created immunity during recent history with infectious diseases such as mumps, chickenpox, polio and measles. Unfortunately, and not until recently, outbreaks of these diseases have started to occur in communities with high levels of anti-vaccination sentiment among their populations. We’ve already seen this with measles in the United States. The virus was declared eradicated there in the year 2000, but anti-vaccination sentiment grew in the years following that, resulting in some populations having high under-immunization rates. In 2019, 1,250 cases of the vaccine-preventable disease were confirmed across several states.
When people are vaccinated — and thus immune — pathogens can’t travel quickly from person to person. It’s much easier and faster (and more ethical, especially because we have the ability) to vaccinate larger groups of people instead of waiting for a pathogen to run its course and infect people naturally before they acquire immunity. Where herd immunity exists, it’s much less likely that those communities will experience outbreaks of a disease. Herd immunity protects everyone, but particularly people who can’t get vaccines for health reasons such as having compromised immune systems.
Now that multiple pharmaceutical companies’ vaccines are being administered across the U.S., discussions about when we could potentially reach herd immunity have been reignited. And a timeline remains somewhat amorphous. According to Dr. Stanley Weiss, an epidemiologist at Rutgers New Jersey Medical School, the percentage of people who’ll need to be vaccinated — and the timeframe in which that can be done — to reach herd immunity are “moving target[s].” This is because infectious variants are emerging that may be more resistant to the vaccine’s immunity.
What If People Don’t Get Vaccinated for COVID-19?
In locations where populations get vaccinated at high rates, a community achieves herd immunity and can eventually eradicate the disease. If a large enough percentage of the population gets the COVID-19 vaccine once it becomes widely available, there won’t be a high enough number of nonimmune people who can spread the virus at high rates. This can keep unvaccinated people safe. We won’t know for sure if enough people get vaccinated until enough doses become available to most of the general population, not just high-risk groups. If a high enough percentage of the population decides they’re not willing to get vaccinated, COVID-19 can continue to spread, particularly if people stop practicing social distancing or wearing masks.

A September 2020 poll from the Pew Research Center found that about half (49%) of those surveyed would “definitely or probably” not get vaccinated against COVID-19. In May of 2020, nearly 72% said that they would get vaccinated. That’s a 21-percentage-point drop, considering that now only 51% of U.S. adults say they “definitely or probably” would get vaccinated. With experts saying 70% to 90% of a population needs to be vaccinated to reach herd immunity, it’s not clear if the United States will be able to achieve this benchmark with its current level of anti-vaccination sentiment. It’s also important to note that people will need to continue getting vaccinated at regular intervals to maintain herd immunity into the future.
What Does Slowing the Spread of COVID-19 Involve?
Until the new vaccines have been deployed and distributed to a large enough percentage of the population, it’s essential to continue doing all we can to slow the spread of the coronavirus. This will prevent us from overtaxing hospital systems and medical resources — and it will save lives. If we sought to achieve herd immunity by virus exposure alone, it would likely mean tens of millions of lives lost and would not guarantee eradication of the virus. The good news, however, is that social distancing, wearing masks, washing hands frequently and taking other similar steps gives us the chance to slow the spread until herd immunity is potentially achieved. The more our population can slow the spread of the virus until a vaccine is in widespread use, the more unnecessary loss of life we can prevent.

Despite what some people may claim, and despite how oddly politicized it’s become, wearing a mask works. A June 2020 study that looked at mask-wearing policies and COVID-19 death rates among 198 countries could not have demonstrated that more clearly. The countries that implemented mask-wearing policies earlier and saw higher compliance rates have had lower mortality rates. With COVID-19 touching almost every area of the world, it’s important to do all we can to limit its spread. Wearing a mask, practicing social distancing, staying home when possible and maintaining good hygiene practices are simple yet effective ways to do just that — and to do your part in keeping our society as safe and healthy as it can be during these unprecedented times.





